THURSDAY, MAY 14
Full-Day Hands-On Digital Dentistry Program
7-Hour Hands-On Course for Doctors
-
This immersive, hands-on program provides a complete, modern digital implant workflow—from virtual surgical planning and guide fabrication to full-arch provisional design and delivery. Using 3Shape Implant Studio, 3Shape Dental Designer, Photogrammetry, and Exocad, participants will gain real-world skills they can immediately implement in clinical practice.
Upon completion of this session, participants will be able to:
Describe and implement a complete digital implant workflow from surgical guide design through full-arch provisionalization, including required hardware, software, scanners, printers, and guided surgery planning protocols using 3Shape Implant Studio.
Design guided surgical appliances and pre-operative and immediate-load provisional restorations using proper digital design parameters to achieve strength, accuracy, and esthetic outcomes.
Select materials and execute 3D printing and post-processing protocols for guides and provisionals, including printer settings, support strategies, curing, finishing, and accuracy verification.
Capture and integrate scan body, MUA, and photogrammetry data and align combined datasets within Exocad to support accurate full-arch digital workflows.
Design and deliver single-unit through full-arch provisional restorations by mating components to Ti-bases and MUAs, selecting connection hardware, and verifying fit, occlusion, and esthetics.
Apply chairside digital workflows to improve clinical accuracy, efficiency, and interdisciplinary communication while reducing errors and increasing case predictability and acceptance.
Participants will finish the session by seating their provisionals on typodont models—verifying fit, occlusion, and design accuracy.
Participative up to 7 hours
AGD Subject code: 690 — Implant Dentistry
-
Dr. Eshraghi received his Bachelor of Science degree from Portland State University in 2002, and both his DMD and Specialty Certificate in Periodontics from Oregon Health and Science University in 2006 and 2009 respectively. Dr. Eshraghi is a Diplomate of the American Board of Periodontology, the highest level of achievement in the field.
He maintains private practices in Beaverton and Tualatin, OR and remains affiliated with OHSU as an assistant clinical professor and actively teaches advanced surgical skills including implant placement. He is passionate about teaching and is pioneering the use of advanced computer aided technologies such as CT scans, CAD/CAM guided surgery, 3D printing and dynamic navigation into the practice of periodontics.
Course Fees
Doctors attending iADS FORUM $1195
Doctors (stand‑alone registration) $1495
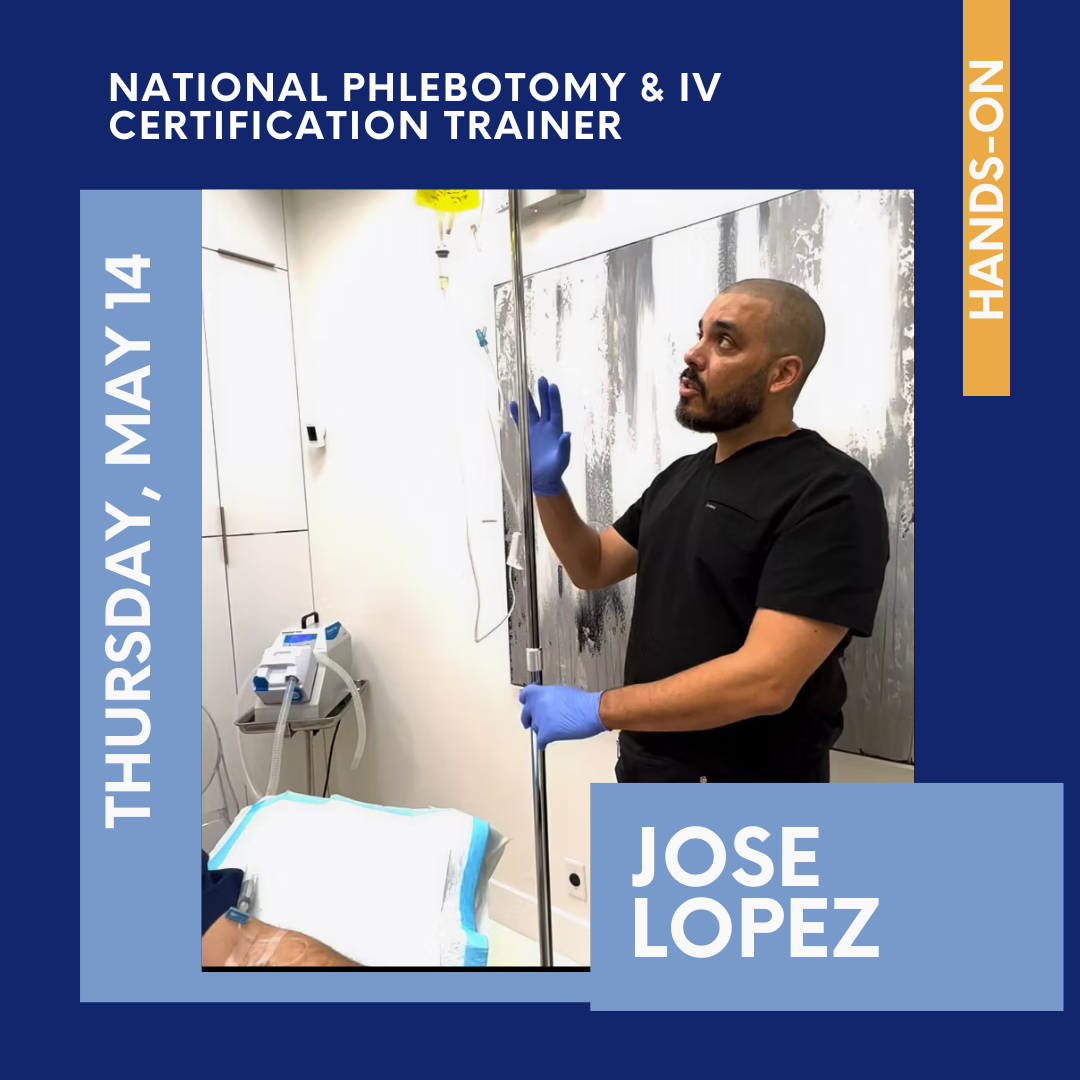
Comprehensive PRF & Phlebotomy Training
4-Hour Hands‑On Course for Doctors & Team Members
-
Unlock the full potential of autologous regenerative medicine in dentistry.
This expanded, integrated program combines Platelet‑Rich Fibrin (PRF) mastery with hands‑on phlebotomy training—designed for doctors and their clinical teams to immediately implement predictable, biologically driven healing protocols.
Participants will gain comprehensive knowledge of A‑PRF, I‑PRF, and Liquid PRF, along with chair side techniques for extraction socket preservation, sinus augmentation, periodontal regeneration, implant therapy, and soft‑tissue enhancement.
This course bridges biology, technique, and team‑based implementation—ensuring you leave confident, competent, and ready to elevate patient outcomes immediately.
Participative up to 4 hours
AGD Subject code: 490 — Periodontics
-
Implement PRF in extraction sites, sinus lifts, periodontal defects, and implant therapy
• Improve healing and reduce complications with autologous growth factors
• Correctly prepare A‑PRF, I‑PRF, and Sticky Bone
• Select appropriate centrifuges, settings, and activation protocols
• Integrate PRF into esthetic and grafting workflows
-
• Perform safe venipuncture with confidence
• Prepare PRF materials chairside
• Troubleshoot clotting and equipment issues
• Support regenerative and surgical workflows
• Begin certification pathways
Course Fees
Doctors attending iADS FORUM $795
Doctors (stand‑alone registration) $995
Auxiliary staff members .................... $395
FRIDAY, MAY 15
Breakfast &Welcome
7:45-8:45
-
In Henry IV, Part 2, Shakespeare penned the famous line, “Uneasy lies the head that wears the crown.” For dental specialists, that unease can feel especially pronounced. Our advanced training prepares us for clinical complexity, but it does not fully equip us for the leadership challenges created by prolonged uncertainty, workforce strain, referral‑relationship pressures, and evolving patient expectations. The tolerance for mistakes feels smaller, the stakes are higher—financially, clinically, and reputationally—and those around us may be grieving the loss of predictability and ease in a profession that has permanently changed. The pressure can be overwhelming.
As a result, we often struggle to know what we should do and how we should show up for our families, colleagues, teams, referring dentists, and patients. The shadow questions—what we should not do, how we should not behave—add an additional layer of stress. At a time when we need a type of support we may never have needed before, and acknowledging that leading through sustained pressure requires a distinct set of skills, where do we turn for guidance? How do we take care of ourselves? What tools help us lead with clarity, steadiness, and resilience in environments where the margin for error is slim and the emotional load is heavy?
Upon completion of this session, participants will be able to:
Describe a practical, sustainable stress‑management philosophy tailored to the realities of modern specialty practice and high‑stakes clinical leadership.
Recognize the role of loss, fatigue, transition, and identity shifts when leading oneself through periods of sustained pressure, clinical complexity, and professional change.
Identify and apply three effective coping strategies for managing anxiety, stress, and decision fatigue—strategies that support both personal well‑being and high‑quality clinical performance.
Develop approaches for maintaining clinical confidence and emotional steadiness in environments where expectations are high, complications carry reputational weight, and leadership responsibilities extend beyond the operatory.
Lecture up to 45 minutes
AGD Subject code: 550 Practice Management and human Relations & 770 Self-Improvement
-
Sreenivas “Sree” Koka was born in the United Kingdom to Indian immigrants and grew up navigating two nationalities, two religions (Anglican and Hindu), two languages (English and Telugu), and two cultures. His diverse upbringing laid the foundation for a dynamic and impactful career in oral healthcare.
Dr Koka has held numerous leadership roles across a broad spectrum of professional settings. His experience includes running a private practice, serving as Department Chair at the Mayo Clinic, working as a prison dentist in Mississippi, and holding academic positions—including Dean at the University of Mississippi Medical Center. He has also served in nonprofit leadership as an Executive Director and led national and international professional organizations. In addition, he contributed his expertise as Chair of MIT’s Sloan School of Management Alumni Board.
Dr Koka is a highly sought-after speaker, having lectured extensively both nationally and internationally. He is one of the few dentists to deliver a TEDx talk and is the co-founder of the Sweet Spot Leader program, which focuses on teaching the human side of leadership to early- and mid-career healthcare professionals. His presentations emphasize the importance of humanity in leadership, team building, and serving underserved communities.
-
Endodontists have much more to offer dental patients that just clean, shape and pack. Dr. Schwartz practices with other specialists and the treatment they provide together is often complex and lengthy. He will conduct a case-based session on decision-making and treatment planning in endodontics, and some of the creative contributions endodontics “brings to the table” in periodontics, prosthodontics, orthodontics and implant dentistry. He will present case histories and lead the audience through the thought process of diagnosis, case selection, and how endodontics can make a significant contribution to the overall treatment plan. In each case he will discuss his rationale and show how he treated the patient. Many long-term recalls will be presented.
Upon completion of this session, participants should be able to:
· Identify how thoughtful endodontic planning and treatment can improve outcomes in restorative dentistry and other dental specialties.
· Explain the role of pre-implant endodontics in comprehensive treatment planning.
· Recognize special clinical situations—including resorption, trauma, and dental anomalies—and describe appropriate endodontic considerations.
Lecture, up to 45 minutes
AGD subject code: 070 Endodontics
-
Dr. Rick Schwartz was a restorative dentist for 19 years prior to entering post-graduate training in endodontics. He attended a 2-year general dentistry residency, and then did a combination of private practice, teaching and dental materials research before entering endodontic training in 1996. He has authored over 100 publications and was a cover author on 3 editions of “Fundamentals of Operative Dentistry” by Quintessence Publishing Co. He is first author of the book “Best Practices in Endodontics”, and is a cover author of “Advanced CBCT for Endodontics”. For the past 28 years he has been in full time private practice limited to endodontics in San Antonio, TX. He has lectured extensively in the U.S. and in 20 other countries.
-
This presentation will deepen your understanding of periodontal phenotype and why this shift in terminology offers an opportunity to “change the game” for diagnosis and interdisciplinary treatment possibilities. I will provide a fresh perspective on gingival recession and introduce Phenotype-Driven Treatment Planning, a recently-published systematic approach to diagnosis, treatment planning, and management of interdisciplinary patients. We will review how you can integrate and apply this information to elevate your teams and practice for the benefit of your patients.
Upon completion of this session, attendees should be able to:
Introduce “periodontal phenotype” and define its clinical parameters.
Discuss the concept of Phenotype Driven Treatment Planning (PDTP) for the interdisciplinary team and patients.
Understand how to utilize and apply these concepts in practice: Case examples with discussion.
Lecture up to 45 minutes
AGD Subject Code: 490 Periodontics
-
Dr. Ashley Hoders has been practicing in and enjoying the Pacific Northwest for over a decade with her husband Jeremy, rescue-pup Rambo, and Hudson, her 4 yr old son. Dr. Hoders is originally from Fort Lauderdale, FL and graduated from the George Washington University, where she was also a Division I All-American Student Athlete (swimming). She subsequently returned to Florida and earned her DMD degree from University of Florida, where she graduated with research.
Dr. Hoders then went on to Baltimore College of Dentistry in Maryland and completed advanced training in general dentistry before entering private general practice in Maryland. Her passion for providing excellent care and building relationships led to the decision to return to school to pursue post-graduate training in both Periodontics and Prosthodontics at the accredited University of Texas Health Science Center in San Antonio. While at the University of Texas, Dr. Hoders became the sixth graduate and first woman to complete this dual specialty program, in which she received specialty certificates in both Periodontics and Prosthodontics and a Masters of Science. She is the first female in the country to hold the distinction of being a Diplomate and Fellow of the American Board of Periodontology as well as the American Board of Prosthodontics. She has contributed to advancing the science of implant dentistry through her published clinical research and continues her involvement with clinical research as a network practice member of the esteemed McGuire Institute. With a passion for interdisciplinary collaboration, she has been active in providing dental education for both dentists and hygienists. Dr. Hoders is the co-founder of SPEAR hygiene and enjoys serving her community as a leader and member of several committees and study clubs at a local and national level.
With her interest in teaching, she also serves as a visiting faculty member in the Department of Periodontology at the University of Washington, is an active member of the American Academy of Restorative Dentistry, and is an ad-hoc reviewer for the Clinical Advances in Periodontics Journal, the Journal of Esthetics & Restorative Dentistry as well as the International Journal of Esthetic and Restorative Dentistry.
Outside of work, Ashley enjoys being a mom and being active, cooking, sommelier training, and time with friends and family.
-
When exploring the physiological boundaries of transverse and anteroposterior dimensions in orthognathic surgery, we are faced with questions of risks and benefits involved. In this lecture we will explore analysis and implementation of this new paradigm. Stability of the various movements will be reviewed, while taking into consideration the impact on the health of the temporomandibular joint. As always, airway will be one of the key considerations of our analysis.
Upon completion of this session, attendees should be able to
Define and differentiate: the multidimensional concepts of maxillomandibular expansion (MME) and maxillomandibular advancement (MMA) in the context of orthognathic surgery.
Analyze and interpret pre- and post-operative airway assessments using virtual surgical planning with drug-induced sleep endoscopy (DISE) to determine airway changes associated with MMA.
Evaluate and formulate treatment strategies for patients with compromised temporomandibular joints (TMJs) to optimize surgical stability and functional outcomes.
Lecture up to 45 minutes
AGD Subject Code: 310 Oral and Maxillofacial Surgery
-
Dr. Reza Movahed is a skilled Oral and Maxillofacial Surgeon, bringing his expertise to patients across the greater St. Louis region, San Francisco Bay area, and beyond. With a focus on treating dentofacial deformities and obstructive sleep apnea, he specializes in corrective jaw surgery, temporomandibular joint procedures, and combined orthognathic and TMJ surgeries.
Dr. Movahed obtained his Doctorate in Dental Medicine from the University of Medicine and Dentistry of New Jersey, followed by residency training at Nova Southeastern University. He further honed his proficiency through a specialized fellowship in TMJ and corrective jaw surgery. He is a Clinical Assistant Professor at Saint Louis University’s Department of Orthodontics. He lectures on surgical orthodontics and actively collaborates on multidisciplinary ortho-surgical cases with residents.
Dr. Movahed is also a prolific writer with contributions to numerous chapters and scientific articles. He is also a coauthor of a textbook focusing on treatments for sleep apnea and dentofacial conditions. Dr. Movahed’s dedication to his craft is rivaled only by his passion for artistic expression; he enjoys painting and making music in his free time.
Dr. Movahed’s patients are consistently amazed by his clinical and compassionate bedside manner. His friendly and approachable personality instantly puts them at ease, fostering an environment of trust and open communication. With his extensive experience and warm demeanor, Dr. Movahed is dedicated to delivering the highest quality of care, ensuring that each patient’s unique needs are met with personalized attention and skillful expertise.
LUNCH 12:00-1:00
-
The midpalatal piezocorticotomy guide is an auxiliary appliance designed to enhance midpalatal piezocorticotomy results. This technique and design, filed under US and Canadian patent applications, provides a novel method for achieving predictable midfacial bone separation. The midpalatal piezocorticotomy technique recommended by the authors involves guide-assisted piezocorticotomy utilizing CBCT-guided planning. This technique enables bilateral separation of the maxillary crests of the palatal processes and the palatine bones. The technique has consistently produced midpalatal suture separation at both the ANS and PNS, along with disjunction of the pterygomaxillary sutures. Our findings consistently demonstrate peri-maxillary suture separation following guided midpalatal piezocorticotomy-assisted MARPE (Microimplant-Assisted Rapid Palatal Expansion) for midfacial expansion. This process involves physiological separation of the frontomaxillary, nasomaxillary, frontonasal, zygomaticomaxillary, and pterygomaxillary sutures in adult patients. These observations suggest that guided piezocorticotomy-assisted midfacial expansion with MARPE operates via a distinct biomechanical mechanism and yields different outcomes compared to surgically assisted rapid palatal expansion (SARPE), which entails direct surgical separation of the midpalatal suture and often includes concomitant Le Fort I osteotomy to facilitate additional maxillary movement.
Upon completion of this session, attendees should be able to:
Become familiarize with the 3d guided midpalatal piezocorticotomy assisted MARPE technique (3D GMP MARPE).
Discuss the benefits and disadvantages of this approach compared to conventional non-guided approach.
Discuss the outcomes of 3D GMP MARPE treatment and its benefits for the upper airway size and treatment of Sleep disordered Breathing/Obstructive Sleep apnea in adults.
Lecture up to 45 minutes
AGD Subject Code: 370 Orthodontics
-
Dr. Koval is a recognized researcher and author with specialized training in occlusion, TMJ disorders, and craniofacial development. Dr. Koval possesses extensive knowledge of direct 3D-printing technologies and currently serves in an Opinion Leadership role regarding the adoption and clinical application of the Graphy Direct Printed Aligners technique. Recognized Opinion Leader for T-Scan applications; Certified in Disclusion Time Reduction (DTR) therapy, a conservative modality for treating Trigeminal Neuralgia and Ménière’s disease. Author of multiple peer-reviewed articles and a book chapter on "T-Scan Digital Occlusal Analysis in Orthodontics" (published in the Handbook of T-Scan Applications, 3rd Edition, 2024). Serves as Principal Investigator for the MARPEFACE project, researching the effects of MARPE and FME on Sleep Disordered Breathing. Published multiple articles researching the effects of 3D Guided Midplatal Piezocorticotomy Assisted MARPE in Adults. Currently enrolled in the Postgraduate Program (2025) to further augment research in medical-dental applications. Dr. Koval practices in Boca Raton, FL, in the practice limited to Airway-focused treatment.
-
Why do technically “perfect” cases sometimes fail? Why do esthetic outcomes collapse, screws loosen, ceramics fracture, or peri-implant tissues deteriorate—despite skilled surgery and careful restoration?
The answer is rarely technique alone. Most complications are established at the planning stage, long before the first incision or impression is made.
In this dynamic, interdisciplinary presentation, Dr. Konrad Meyenberg will reveal how subtle decisions in diagnosis, implant system selection, prosthetic design, and interdisciplinary handoffs determine whether cases remain stable—or slowly fail.
Participants will be introduced to a practical “restorative gap management” framework for evaluating the difference between patient expectations, biological limitations, existing anatomy, and prosthetic feasibility. Through carefully selected clinical cases, Dr. Meyenberg will guide attendees through real-world decision trees across orthodontics, periodontics, oral surgery, endodontics, and prosthodontics.
A unique focus of this session is the often-overlooked engineering and biomechanical differences among implant systems. Clinicians frequently choose implant platforms based on familiarity, training background, price, or influence—without understanding how connection design, component tolerances, surface characteristics, and load transfer directly affect complication rates, esthetic stability, and long-term success.
This lecture is designed to elevate the biomechanical literacy of all specialists and provide a shared interdisciplinary language that improves planning, communication, and outcomes—before complications ever occur.
Upon completion of this session, attendees should be able to:
Recognize how prosthodontic “gap management” influences the choice between orthodontics, additive bonding, ceramic restorations, fixed bridges, or implant therapy in the esthetic zone.
Identify the critical planning decisions that most often lead to esthetic failure and technical complications, including implant positioning, soft-tissue limitations, abutment design, emergence profile, and occlusal strategy.
Differentiate key engineering and biomechanical features of implant systems—such as connection design, component precision, surface treatments, and load distribution—and explain how these variables influence mechanical stability and biological response.
Select predictable restorative strategies for endodontically treated teeth by evaluating remaining tooth structure, ferrule, post indications, and fracture risk within an interdisciplinary context.
Apply a repeatable interdisciplinary workflow for diagnosis, prosthetically driven planning, provisionalization, and definitive restoration that improves predictability, reduces remakes, and minimizes mechanical and biological complications.
Why All Specialists Should Attend
Whether you place implants, restore them, manage peri-implant tissues, move teeth, preserve compromised teeth, or design prostheses, your decisions influence outcomes far beyond your own specialty.
This course provides:
A shared interdisciplinary decision framework
A deeper understanding of implant system engineering and biomechanics
Practical strategies to prevent the most common technical and esthetic failures
Clinical insights that immediately improve daily practice
Lecture up to 45 minutes
AGD Subject Code: 370 Orthodontics
-
Konrad H. Meyenberg graduated at the University of Zurich, Switzerland in 1985. He completed a 4-year post-graduate program in reconstructive dentistry in Zurich at the department for fixed and removable prosthodontics and material sciences (chairman: Prof. Peter Schärer).
Dr. Meyenberg is a certified specialist for Reconstructive Dentistry of the Swiss and European Dental Society (specialty degree since 1993). He also has a private practice limited to esthetic reconstructive dentistry and implantology in Zurich, Switzerland.
He is a senior lecturer for reconstructive dentistry at the Universitis of Zurich, Dental Schools. Since 1990, he has been a well-known speaker at numerous international congresses and events, having presented at more than 500 congresses. Reviewer of numerous scientific journals.
-
This session provides a clear and accessible overview of how modern artificial intelligence systems work and how these foundations translate into practical tools used across dentistry and healthcare. Attendees will learn core AI concepts and how its growing capabilities are shaping dentistry. We will explore clinical applications such as imaging interpretation, periodontal and implant planning, diagnostic support, and risk prediction, as well as AI’s role in accelerating new therapy development. Participants will also learn how AI enhances workflow efficiency, clinical management, and patient outcomes, with a focus on practical use, limitations, and responsible integration.
Upon completion of this session, attendees should be able to:
Explain essential AI concepts (e.g., datasets, training, algorithms, model limitations) and describe how these models are used in dentistry.
Identify key areas where AI is currently applied in dentistry, including imaging interpretation, digital treatment planning, risk assessment, and workflow automation.
Recognize the benefits and limitations of AI, enabling informed decision-making when integrating new technologies.
Discuss how AI is reshaping healthcare delivery for providers, patients, and administrators, and anticipate future directions for interdisciplinary specialty care.
Lecture up to 45 minutes
AGD Subject Code: 149 Multidisciplinary Topics
-
Dr. Nathalia Andrade, DDS, PhD, is a clinician–scientist and Clinical Assistant Professor of Periodontics at the University at Buffalo School of Dental Medicine. Her work integrates advanced periodontal and implant therapy with cutting-edge digital and artificial intelligence technologies. Dr. Andrade directs UB’s Periodontal and Dental Technologies curriculum, collaborates with engineering and data-science teams on AI-driven genetic therapy discovery, and leads initiatives that advance AI innovation in dental education. Her research focuses on leveraging machine learning, digital workflows, and simulation-based training to enhance clinical decision-making, improve surgical precision, and elevate patient outcomes.
-
This lecture introduces new concepts, new technology, and new surgical techniques associated with the use of wedge-shaped implants, which allow to exploit native bone by combining Leonard Linkow and P.I. Bränemark’s teachings with the advantages of piezoelectric microsurgery developed by the author.
Upon completion of this session, attendees should be able to:
Understand the concept of bone volume adequacy in relation to implant dimensions as a prerequisite for implant success;
Understand how piezolectric osteotomies and non-circular implant sites allow to place implants exclusively in native bone even in severely atrophic cases
Understand the differences in peri-implant bone response to screw- vs wedge-implant site preparation.
Lecture up to 45 minutes
AGD Subject Code: 310 Oral and Maxillofacial Surgery
-
Tomaso Vercellotti, MD, DDS is the inventor of piezoelectric bone surgery and co-inventor of Rex PiezoImplants.
He has authored some of the most important scientific and clinical studies on piezoelectric bone surgery as well as the books Essentials in Piezosurgery: Clinical Advantages in Dentistry
(Quintessence, 2009) and Piezoelectric Bone Surgery: A New Paradigm (Quintessence, 2020).
Dr. Vercellotti is Founder and first President of the International Piezoelectric Bone Surgery Academy (IPA), and Honorary Professor and Faculty at the University College of London Eastman Dental Institute. He is an active member of numerous professional associations and has dedicated over 30 years to the rehabilitation of complex cases, currently maintaining a private practice specializing in periodontology and implantology in Genoa, Italy.
-
This fast-moving scientifically based presentation will cover cutting edge tips, tricks and techniques to “Make MY Job Easy” and make me look good while ensuring ideal patient care. Restorative Dentists have many Specialists to chose from, learn what you must provide to make your practice unique and become the Goto practice for Dental Implant Referrals. Rather than relying on donuts and dinner parties we will dive into the Technology, Procedures, Communication and “gifts” that matter most. As a GP in an all Implant Restorative practice for over 30 years my referral patterns have been fine tuned to work with Specialists that know what I need and provide it routinely…so can you!
Upon completion of this session, attendees should be able to:
Identify the clinical, technological, and communication elements specialists value most when selecting restorative partners for implant referrals.
Describe specific systems, procedures, and workflows that position a restorative practice as a reliable and preferred referral destination for implant cases.
Apply practical strategies—beyond traditional relationship-building tactics—to enhance collaboration, efficiency, and patient outcomes in interdisciplinary implant care.
Lecture up to 45 minutes
AGD Subject Code: 690 Implant Dentistry
-
Dr. Vogel graduated from Columbia University College of Dental Medicine in New York City before completing residency training at Jackson Memorial, Mount Sinai and Miami Children’s Hospitals in Miami Florida.
His practice is focused on Implant Prosthetics and Reconstructive Dentistry working as a team member with several specialists providing implant-based comprehensive treatment, conducting clinical trials and providing clinical advice to the dental implant field. Dr. Vogel has developed and collaborated on the development of several components and techniques currently in use in Implant Dentistry.
Dr. Vogel lectures internationally on Implant Dentistry focusing on Precision and Predictability through ideal planning, use of digital technologies and team interaction. He has published over forty scientific articles, is a Fellow of the International Team for Implantology, a Diplomat and Fellow of the Academy of Osseointegration and Fellow of the International College of Dentists.
PROGRAM CONCLUDES 5:15
Saturday, MAY 16
Breakfast & Welcome
7:45-8:45
-
Details Coming Soon!
Lecture up to 45 minutes
-
Lyndon F. Cooper, D.D.S., Ph.D., is dean of VCU School of Dentistry and an internationally renowned and innovative patient-oriented researcher and clinician. He has established a reputation for leading innovative teams in translational research and advancing a research-oriented approach to evaluating clinical devices and other patient-care solutions.
Prior to joining VCU, Cooper served as associate dean for research and head of the Department of Oral Biology at University of Illinois Chicago (UIC) School of Dentistry. Here, he expanded research in regenerative sciences, innovative biomedical devices and translational studies evaluating the roles of a variety of biomarkers linked to cancer. Under Cooper’s leadership, the Department of Oral Biology at UIC served as a foundation for many of the basic science topics taught to the school’s D.M.D., M.S., and Ph.D. students. He continued his clinical activities as a prosthodontist by leading clinical studies and establishing the school’s Clinical Research Center.
Prior to UIC, Cooper served as program director of Advanced Prosthodontics and Stallings Distinguished Professor at the University of North Carolina Adams School of Dentistry. He is a Diplomate of the American Board of Prosthodontics (ACP) and a former ACP President, who received the ACP’s 2004 Clinician/Researcher Award. He was also named the recipient of the 2009 International Association for Dental Research Distinguished Scientist Award for Prosthodontics and Implantology.
After earning his D.D.S. from New York University, Cooper went on to earn a Ph.D. from the University of Rochester, New York, and a Certificate in Prosthodontics from the Eastman Dental Center in Rochester. Later, he completed a two-year research fellowship at the National Institute of Dental and Craniofacial Research in Bethesda, Maryland.
-
Led by Eric Rindler, this program brings two interdisciplinary teams together to walk through real-world cases using a 360-degree approach to treatment planning. Participants will examine cases from biological, functional, esthetic, and financial perspectives, gaining insight into how collaborative planning across specialties leads to clearer decision-making, stronger case sequencing, and more predictable outcomes.
Upon completion of this program, participants will be able to:Utilize a comprehensive, interdisciplinary framework for treatment planning that integrates biology, function, esthetics, and financial considerations.
Analyze real-world cases to understand how collaboration across specialties influences sequencing, predictability, and long-term success.
Identify practical communication strategies that support alignment among providers and improve patient understanding of complex treatment plans.
Lecture up to 80 minutes
-
Dr. Eric Rindler received his DDS from the University of Texas Health Science Center in San Antonio Texas, his Certificate in Periodontics from the University of Missouri, Kansas City School of Dentistry, and his MBA from Texas McCombs School of Business. He is founder and CEO of Intelibly, has held the position of Associate Professor at UTSHCSA in General Dentistry and has served as a Guest Instructor at the Kois Center in Seattle, Washington. Dr. Rindler maintains a private practice Limited to Periodontics and Dental Implants in San Antonio, Texas.
-
With the right messages and communication training, you can deliver memorable sound bites to people you meet in everyday life to capture their attention and educate them about your specialty. This webinar builds on my original iADS research and the resulting “elevator pitches.” This concise, cogent presentation gives you 15-second messages that you and your team can deliver to a public. Join me as we go on an adventure out of the office to enlighten many people who don’t know what they don't know about your specialty. Train your team to educate people in a friendly, engaging, and helpful manner. You will discover new patients hiding in plain sight who will be grateful for the treatment you provide.
Upon completion of this session, attendees should be able to:
Identify the key words and phrases to engage people in conversation and about specialty care.
Have 15-second “sound bites” at the ready to efficiently communicate the benefits of specialty treatment.
Have a practical plan to train their team to enlighten the public about your specialty.
Lecture up to 15 minutes
AGS Subject code 550, Practice Management & Human Relations
-
David Schwab, Ph.D., is a professional seminar speaker and consultant. He is the author of The Dental Communication Advantage: Proven Scripts to Train Your Team and Grow Your Practice. He has served as Director of Marketing for the American Dental Association and Executive Director of the American College of Prosthodontists. He provides lectures, online training, and in-office consulting with a focus on specialty practices. Dr. Schwab holds a Ph.D. in English from Northwestern University.
-
Artificial intelligence is no longer emerging—it's here, reshaping how dentists diagnose, document, and communicate with patients. And increasingly, it's how insurance companies review claims. Drawing on experience in FDA and CMS policy development and current leadership at Overjet, global leading dental AI company with multiple FDA clearances, this session cuts through the hype to address what clinicians actually need to know.
We'll demystify FDA clearance—what it requires, what it doesn't, and how to distinguish rigorously validated tools from marketing claims. We'll explore how AI detects subtle radiographic changes that are difficult to perceive, supports longitudinal disease tracking, and generates evidence-based documentation that can strengthen insurance approvals. You'll see how AI becomes the connective tissue of a modern practice: from first patient impression, through clinical conversation with color-coded visuals, to post-visit follow-through.
Early adopters report reduced decision fatigue, streamlined documentation, and improved case acceptance. But successful implementation requires more than software—it demands calibration, team training, and thoughtful change management. We'll also address data governance, transparency, and clinician oversight so you can adopt responsibly.
By engaging critically with these tools now, you position your practice for sustainable success—and gain the knowledge to shape the policy conversations that will define AI's future in dentistry.
Upon completion of this session, attendees should be able to:
Explain FDA clearance requirements for dental AI, including performance validation, risk classification, and post-market surveillance.
Describe how AI detects subtle radiographic findings and supports longitudinal disease tracking to strengthen clinical decision-making.
Identify how AI-generated documentation can improve insurance claim approvals and recognize that payers are increasingly using AI too.
Apply AI-powered visualization tools to enhance patient communication, shared decision-making, and case acceptance.
Evaluate implementation requirements—including calibration, team training, and change management—for successful AI adoption.
Assess principles of data governance, transparency, and clinician oversight essential for responsible AI integration.
Lecture up to 30 minutes
AGS Subject code 550, Practice Management & Human Relations
-
Dr. Natalia Chalmers is a board-certified pediatric dentist and 2025 AAPD Pediatric Dentist of
the Year, oral health policy expert, and public health advocate bringing over 20 years of clinical,
research, and regulatory experience to the forefront of dental innovation. As the Chief Dental
Officer and Head of Clinical Innovation at Overjet, she leverages data-driven insights to
transform dental healthcare delivery and ensure access to high-quality, patient-centered care.
Previously, Dr. Chalmers made history as the first Chief Dental Officer in the Office of the
Administrator at the Centers for Medicare & Medicaid Services (CMS). There, she led
groundbreaking initiatives to expand dental coverage, established the first CMS dental claims
processing system, and implemented new quality measurements that reshaped the national
conversation on oral health. Her public sector leadership also includes tenure as a Dental
Officer at the US Food and Drug Administration (FDA).
A recognized expert in clinical analytics, Dr. Chalmers is dedicated to advocating for the role of
health policy across the lifespan—viewing dental well-being as intrinsic to whole-person care.
Dr. Chalmers completed her Doctor of Dental Surgery degree at the Faculty of Dental Medicine
of the Medical University of Sofia, a residency in pediatric dentistry at the University of Maryland
School of Dentistry, and a Ph.D. in oral microbiology from the Graduate Partnerships Program
of the University of Maryland School of Dentistry and the National Institute for Dental and
Craniofacial Research at the National Institutes of Health, Post-doctoral Fellowship at the ADA
Forsyth Institute, and Clinical Research Fellowship at the National Institute for Dental and
Craniofacial Research, National Institutes of Health. Dr. Chalmers holds a Master’s degree in
Clinical Research from Duke Medical University and a Certificate in Drug Development and
Regulatory Science from the University of California, San Francisco School of Pharmacy.
LUNCH 12:30-1:30
-
Sometimes the smallest cases spark the biggest insights. Dr. Tucker, along with a panel of specialists, will present concise, focused cases that highlight unique clinical dilemmas and invite interactive, interdisciplinary problem-solving. Through guided discussion and shared perspectives, participants will explore how collaborative thinking can elevate decision-making and lead to more predictable treatment outcomes.
Upon completion of this session, participants will be able to:Recognize key decision points in smaller or seemingly straightforward cases that benefit from interdisciplinary input.
Apply collaborative problem-solving approaches to resolve clinical dilemmas and strengthen treatment planning decisions.
Lecture, up to 20 minutes
AGD subject code 149 multidisciplinary topics
-
Dr Stephen Rimer received his BDS (Bachelor of Dental Science) degree from the University of Witwatersrand, Johannesburg, South Africa. He did his post graduate education in the United States at Michael Reese Hospital in Chicago and the University of Miami Medical School at Jacksonville Memorial Hospital in Miami. He completed a fellowship in orthognathic surgery and reconstructive jaw bone surgery at the University of Miami and maintains a private practice in oral maxillofacial surgery in Boca Raton, Florida.
Dr Rimer is board certified and has practiced in Boca Raton since 1983. He has lectured nationally and internationally. His specific area of interest and expertise is reconstructive jaw surgery [Orthognathic Surgery] for patients who have grown or developed incorrectly or as a result of trauma or surgical defects. He is also recognized as a leader in the field of bone grafting, SFOT and dental implantology.
Dr Rimer is specifically recognized for his understanding of interdisciplinary treatment planning as it relates to complex cases which require a multi-disciplinary team approach including plastic and reconstructive surgery, orthodontics, restorative and all other dental specialist and their inter-relationship with oral and maxillofacial surgery. To this end, he founded the D.E.A.L. (Dental Excellence, Advancement and Learning) Study Club 26 years ago to help coordinate treatment amongst his colleagues of these kinds of difficult cases and to help educate all members of the team as to the possibilities available in managing complex patient care.
His office has an unusual association with a Master Dental Technichian, a key member of any case planning.
In recognition of his diagnostic and treatment planning expertise, he was awarded the very special “Saul Schluger Award” in 2012 for Excellence in Comprehensive Care and Clinical Treatment Planning.
Dr. Rimer is a member of the American Academy of Esthetic Dentistry which is limited to the top 100 worldwide leaders in Esthetic Dentistry. He is one of very few Oral and Maxillofacial Surgeons to be a member of this group.
He spends his free time doing wildlife photography amongst other activities.
Together with his son,he also runs a specialized Safari Travel company, Journeys Unforgettable. He is married, has 2 children and lives in Boca Raton.
-
For ideal preservation of teeth, regrowth of alveolar bone after periodontal disease, cancer and/or trauma and for future placement of endosseous dental implants, bone regeneration is required. Whether or not a patient is systemically challenged in terms of osseous healing, there is often the desire to optimize the predictability of vital bone growth, not just volume preservation. To obtain the maximal amount of vital bone and volume in the shortest time, the incorporation of a bioactive barrier and/or growth enhancing materials into the graft mixture which have inherent bioactive factors can assist in this process. In contrast to PRP, in vitro assays and in vivo results have shown that L-PRF will release growth factors like β-TGF, PDGF, IGF and more over a course of 28+ days. DFDBA fibers have some osseoinductivity and give bone graft materials the ability to hold their shape. Amnion-chorion membranes have been incorporated in orthopedic, neurosurgery and dento-alveolar surgery for their anti-infective, osteogenic and angiogenic properties. Platelet derived growth factor can increase the predictability for periodontal as well as alveolar bone and soft tissue regeneration. Clinical cases validated with literature and histology will show how these materials can increase vital bone formation and decrease the risk of future periodontal and peri-implant diseases.
Upon completion of this session, attendees should be able to:
Evaluate the biological rationale for using bioactive barriers and growth-enhancing materials to optimize vital bone regeneration in periodontal, traumatic, and implant-related defects.
Differentiate the regenerative roles and clinical advantages of L-PRF, DFDBA fibers, amnion-chorion membranes, and platelet-derived growth factors in achieving predictable bone and soft tissue outcomes.
Apply evidence-based protocols for combining graft materials and biologics to enhance vital bone formation, reduce healing time, and decrease the risk of future periodontal and peri-implant disease, as demonstrated through clinical cases and histologic validation.
Lecture up to 30 minutes
AGS Subject code 690, Implants
-
Dr. Robert A. Horowitz graduated from Columbia University School of Dental and Oral Surgery in 1982. After completing one year in general practice, he finished a 2-year training program in Periodontics at New York University and the Manhattan VA Hospital. In 1996, Dr. Horowitz completed a 2-year fellowship program in Implant Surgery at New York University concentrating in bone grafting procedures.
As Clinical Assistant Professor in Periodontology and Implant Dentistry at New York University since 1996, he teaches and conducts research in bone grafting and other topics related to periodontics and implant dentistry, and conducts research in the areas of Biomaterials and Biomimetics, Oral Diagnosis/Oral Pathology/Oral Medicine.
Dr. Horowitz has published over 60 papers and a book chapter, has lectured and taught hands-on courses both nationally and internationally, and has performed research in periodontal regeneration, perio-plastic surgery, bone grafting, extraction socket augmentation, growth factors/enhancers and the placement of dental implants in areas of limited available bone.
-
The purpose of this webinar is to educate doctors on the critical aspects of understanding and evaluating dental groups with information that will empower them to make more informed decisions for their future. When a doctor considers options for the future, there are 3 primary paths to consider: 1) selling your practice to another doctor, 2) selling to a DSO (Dental Support Organization), or 3) partnering with a DPO (Dental Partnership Organization).
Practice sales to other doctors or DSOs typically involve doctors who are later in their career. However, the DPO model is quite different and designed for doctors at just about any stage of their career. The DPO model can be a very appealing option for doctors who want to maintain the feel, culture, and controls of private practice, but also want the support, expertise, and potential financial upside that a group provides.
In this webinar we will explore key criteria such as doctor autonomy, financial considerations, legal details, deal structure parameters, and new innovations that can improve the outcome for doctors. Attendees will learn about EBITDA and valuations, arbitrage, and different business models for groups. This course is densely packed with useful information that is relevant for doctors at every stage of their career.
Upon completion of this session, attendees should be able to:
Understand how to maximize the financial value of your practice.
Explore the pros and cons of the DSO model vs. the DPO model.
Review important legal and financial deal structure items when considering a DSO or DPO.
Lecture up to 30 minutes
AGS Subject code 550 Practice Management and Human Relations
-
Ian McNickle, MBA serves as CEO (Chief Executive Officer) and Board Member for Icon group. He is responsible for the primary design and innovations in ICON's unique Dental Partnership Organization (DPO) business model.
Ian is an experienced business executive and entrepreneur who has helped build several successful companies in the dental industry. Prior to leading ICON, he helped launch and build The DSO Project, and WEO Media, a 4X “Best of Class” award-winning dental marketing agency.
While President of The DSO Project, Ian worked alongside Jeromy Dixson, DMD, MBA to advise doctors in all aspects of DSO development in order to help doctors develop, scale, fund, and optimize their DSO. This experience helped build the foundation for ICON.
In addition, Ian was a Co-Founder and Partner at WEO Media, a four-time award winning “Best of Class” dental marketing agency. Under his leadership WEO Media quickly grew to become one of the largest and most widely respected dental marketing firms in North America, and has garnered an impressive list of industry endorsements and awards. Founded in 2009, WEO Media has grown to nearly 50 employees and has provided marketing services for over 2,000 general dental and specialty practices.
Ian is a nationally recognized expert on dental practice / DSO marketing and growth. He has developed significant expertise in all aspects of dental marketing, growth strategy, business development, operations, executive management, and related topics. Ian recently published his first book titled "Mastering Practice Growth – The Definitive Guide to Growing Your Dental Practice or Group" which provides dentists a detailed roadmap to grow their practice or group.
Ian has been named a Top CE Leader and Consultant by Dentistry Today for the last five consecutive years.
Ian has a BS in Mechanical Engineering from Washington State University where he was also a graduate of the University Honors Program. In addition, he graduated Cum Laude with an MBA from the University of Washington.
-
Details Coming Soon
Lecture up to 30 minutes
AGS Subject code 149 multi-disciplinary topics
-
Dr. Jay Patel is an Assistant Professor of Health Informatics and Dentistry at Temple University Kornberg School of Dentistry. Dr. Patel is a dentist, informaticist, and clinical scientist, and he holds a Master's and PhD in Informatics. Dr. Patel's research endeavors revolve around the strategic utilization of vast electronic health record data (EHR) and the application of artificial intelligence (AI) methods to improve patient care and outcomes. His primary focus is developing prediction models that accurately assess the risk of initiation and progression of dental diseases and understand oral health disparities. By identifying high-risk patients and social determinants of health factors in vulnerable populations, Dr. Patel aims to enhance preventive measures, promote proactive dental healthcare practices, and reduce oral health disparities. In addition to his expertise in EHR analysis, Dr. Patel also has expertise in phenotyping dental diagnoses through state-of-the-art informatics methods such as natural language processing and machine learning models through EHR data. Dr. Patel has also developed numerous clinical decision support and learning health systems. These cutting-edge tools are designed to foster data-driven practices, empowering healthcare professionals to make informed decisions and significantly elevate the quality of patient care and reduce health disparities. Dr. Patel's visionary approach has proven instrumental in bridging the gap between medical and dental care, improving health information exchange between providers, and facilitating the utilization of harmonized datasets for clinical research, patient care and quality improvement.
-
This presentation explores the evolving paradigm shift in implant dentistry from a bone-centric approach to one that prioritizes soft tissue health, stability, and esthetics. Participants will examine how peri-implant soft tissue management influences long-term implant success, patient outcomes, and clinical decision-making, supported by current evidence and clinical concepts.
Upon completion of this session, attendees should be able to:
Compare traditional bone-driven implant protocols with contemporary soft tissue–focused treatment concepts.
Identify key soft tissue parameters that impact peri-implant health, esthetics, and long-term stability.
Apply innovative treatment strategies to optimize long-term functional and esthetic clinical outcomes.
Lecture up to 45 minutes
AGS Subject code 550 Practice Management and Human Relations
-
Dr. Boltchi received his dental degree from the Medical University of Hannover in Germany and a Certificate in Periodontics associated with a Master of Science degree in Oral Biology from Baylor College of Dentistry in Dallas, Texas. Dr. Boltchi is a faculty member of Spear Education and CDOCS, and also maintains a full-time private practice in Periodontics and Dental implants in Dallas-Fort Worth, Texas. Dr. Boltchi has achieved Board Certification status with the American Board of Periodontology and is a fellow of the International Team for Implantology (ITI).